The Spread of Antibiotic Resistance: A Growing Global Crisis
The world is facing a silent pandemic, one that threatens to unravel decades of progress in public health: the rise of antibiotic-resistant bacteria. This escalating crisis poses a profound threat to global health security, jeopardizing the effective treatment of common infections and casting a long shadow over the future of medicine. The implications extend far beyond the individual, impacting healthcare systems, economies, and societal stability.
The Escalating Threat
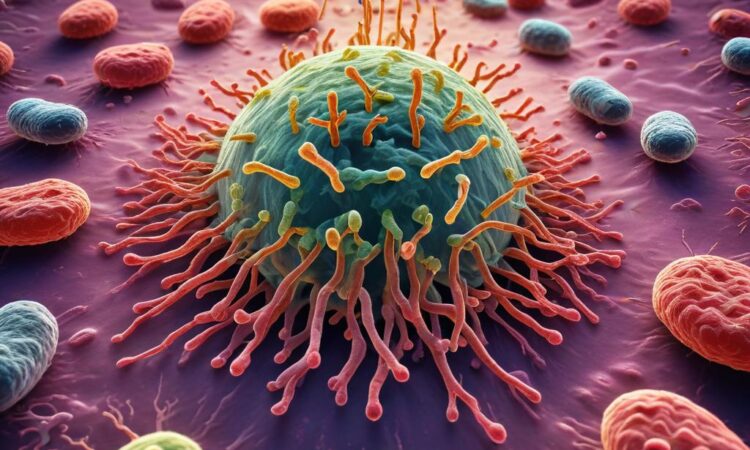
Antibiotics, once miracle drugs, are losing their effectiveness. Overuse and misuse, coupled with the inherent ability of bacteria to evolve, have fueled the emergence of antibiotic-resistant strains. These \”superbugs\” are capable of withstanding even the most potent antibiotics, rendering infections untreatable and leading to prolonged illnesses, increased mortality, and substantial healthcare costs. The consequences are particularly devastating in low- and middle-income countries, where access to effective antibiotics is often limited and healthcare systems are already strained.
The mechanisms of antibiotic resistance are complex and multifaceted. Bacteria can develop resistance through various strategies, including mutations that alter the target site of the antibiotic, enzymatic inactivation of the antibiotic, and the development of efflux pumps that actively expel the drug from the bacterial cell. The spread of resistance genes, often mediated by mobile genetic elements such as plasmids, further exacerbates the problem, allowing resistance to rapidly disseminate among bacterial populations.
The Role of Antibiotic Use
The overuse and misuse of antibiotics are major drivers of antibiotic resistance. In many settings, antibiotics are prescribed inappropriately, for viral infections where they are ineffective, or for too short a duration. The widespread use of antibiotics in agriculture, particularly in livestock farming, further contributes to the problem by creating a selective pressure that favors the survival and proliferation of resistant bacteria. These resistant bacteria can then spread to humans through direct contact or through the food chain.
The agricultural use of antibiotics raises significant ethical and public health concerns. The practice of routinely administering antibiotics to livestock as growth promoters creates a breeding ground for resistant bacteria. These resistant strains can then be transmitted to humans through various routes, including the consumption of contaminated meat and exposure to animal waste.
The Impact on Healthcare
The rise of antibiotic resistance is placing an immense strain on healthcare systems worldwide. Treating infections caused by resistant bacteria requires more expensive and less effective therapies, leading to prolonged hospital stays, increased healthcare costs, and higher mortality rates. The lack of effective treatment options also forces healthcare professionals to resort to older, more toxic antibiotics, which can have significant side effects.
The economic burden of antibiotic resistance is substantial. The costs associated with treating resistant infections, lost productivity, and increased mortality represent a significant drain on national economies. The World Health Organization (WHO) has estimated that the economic impact of antibiotic resistance could reach trillions of dollars annually if effective interventions are not implemented.
The Urgent Need for New Strategies
Combating the global crisis of antibiotic resistance requires a multi-pronged approach encompassing various strategies. The development of new antibiotics is crucial, but this is a complex and expensive undertaking. The pipeline of new antibiotics is dwindling, highlighting the urgent need for increased investment in research and development. Moreover, strategies to optimize antibiotic use, including improved diagnostics and stewardship programs, are essential to slow the emergence and spread of resistance.
Antibiotic stewardship programs aim to promote the judicious use of antibiotics, ensuring that they are used only when necessary and at the appropriate dose. These programs involve a combination of educational initiatives, improved infection control practices, and the implementation of guidelines for antibiotic prescribing. By reducing unnecessary antibiotic use, these programs can help slow the emergence and spread of resistance.
Investing in the development of new diagnostic tools is also critical. Rapid and accurate diagnostic tests can help ensure that antibiotics are used only when they are needed, reducing the risk of contributing to antibiotic resistance. These tests can also help identify the specific bacteria causing an infection, allowing for the selection of the most appropriate antibiotic, thus improving treatment outcomes.
Beyond Antibiotics: Innovative Approaches
The search for alternatives to traditional antibiotics is also gaining momentum. Researchers are exploring various strategies, including the development of new antimicrobial therapies that target bacterial virulence factors, rather than killing the bacteria directly. This approach can reduce the selective pressure for the development of resistance.
Phage therapy, the use of bacteriophages (viruses that infect bacteria) to treat bacterial infections, is another promising area of research. Phages have a long history of use in some parts of the world and are showing potential as a novel therapeutic approach. However, more research is needed to fully understand their safety and efficacy.
Other innovative approaches include the development of new vaccines to prevent bacterial infections, the use of probiotics to restore the balance of the gut microbiota, and the exploration of novel antimicrobial peptides.
Societal Implications
The societal impact of untreatable infections extends far beyond the individual level. The rise of antibiotic resistance threatens to undermine the progress made in modern medicine, jeopardizing the success of complex surgical procedures, organ transplantation, and cancer treatments, all of which rely on the ability to effectively combat infections. The economic burden on healthcare systems and societies as a whole will be immense, potentially leading to increased healthcare disparities and social instability.
The threat of antibiotic resistance necessitates a global collaborative effort. International cooperation is essential to share best practices, coordinate research efforts, and implement effective strategies to combat this growing crisis. This requires a concerted effort by governments, healthcare professionals, researchers, and the public to ensure the responsible use of antibiotics and promote the development of new treatments and prevention strategies. Failure to act decisively will have far-reaching and potentially catastrophic consequences for global health security.
The challenge of antibiotic resistance requires a paradigm shift in how we approach infectious diseases. It demands a commitment to responsible antibiotic use, investment in research and development, and the implementation of effective stewardship programs. Only through a collaborative and multi-faceted approach can we hope to avert the looming threat of a post-antibiotic era.
The future of healthcare depends on our ability to effectively address the challenge of antibiotic resistance. It is a challenge that requires immediate attention and concerted global action to prevent a return to a time when even minor infections could be fatal.