Impact of Climate Change on Disease Vectors: An In-Depth Examination
Climate change, driven primarily by anthropogenic greenhouse gas emissions, is profoundly altering global ecosystems. One of the most significant and often overlooked consequences is the impact on the spread of infectious diseases. Changes in temperature, rainfall patterns, and the geographic distribution of disease vectors – organisms like mosquitoes, ticks, and rodents that transmit pathogens – are creating new challenges for public health worldwide.
Temperature: A Key Driver of Disease Transmission
Temperature plays a crucial role in the lifecycle and reproductive capacity of many disease vectors. Increased temperatures can accelerate the development and reproduction rates of mosquitoes, for example, leading to larger populations and an increased risk of transmission for diseases like malaria, dengue fever, Zika virus, and West Nile virus. Warmer temperatures can also expand the geographic range of these vectors, allowing them to thrive in previously unsuitable environments. This expansion exposes previously unaffected populations to these diseases, placing a strain on healthcare systems and potentially leading to widespread outbreaks.
Conversely, some vector-borne diseases are sensitive to extreme heat. While moderate warming can benefit some vectors, excessively high temperatures can be lethal or inhibit reproduction. Understanding these complex temperature-dependent relationships is critical for accurate predictions of future disease risks.
Rainfall and Humidity: Amplifying the Effect
Rainfall patterns are also intimately linked to the spread of vector-borne diseases. Increased rainfall can create ideal breeding grounds for mosquitoes, particularly in stagnant water sources like puddles, ditches, and artificial containers. Heavy rainfall can also lead to flooding, which disrupts sanitation systems and creates environments conducive to the proliferation of disease vectors. Conversely, droughts can concentrate populations of vectors in remaining water sources, increasing the risk of transmission. Furthermore, higher humidity levels, often associated with increased rainfall, can create a favorable environment for the survival and spread of disease-causing pathogens.
The interplay between temperature and rainfall is particularly significant. A warmer climate often leads to more intense rainfall events, creating a synergistic effect that enhances the risk of disease outbreaks. Predicting these complex interactions requires sophisticated climate modeling and epidemiological studies.
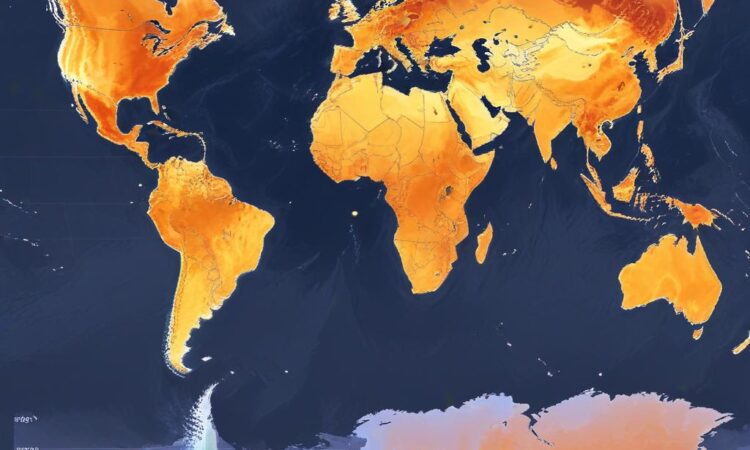
Changes in Vector Range: Expanding the Threat
One of the most alarming aspects of climate change’s impact on disease vectors is the potential for range expansion. As temperatures rise and climates shift, disease vectors are able to migrate to higher altitudes and latitudes, expanding their geographical reach. This phenomenon introduces pathogens into new areas, where populations may lack immunity and healthcare infrastructure may be inadequate to respond to outbreaks. For instance, the northward expansion of mosquito-borne diseases into previously unaffected regions of Europe and North America is a growing concern.
This expansion is not solely determined by temperature. Factors such as changes in vegetation, land use, and human migration also play a role in shaping the distribution of vectors. Understanding the complex interplay of these factors is vital for effective disease surveillance and prevention strategies.
The Impact on Human Health: A Global Perspective
The combined effects of temperature, rainfall, and vector range expansion have significant implications for global public health. Increased incidence of vector-borne diseases can lead to higher rates of morbidity and mortality, placing a substantial burden on healthcare systems. The economic consequences can be equally devastating, as outbreaks can disrupt economic activities, tourism, and agricultural production.
Vulnerable populations, particularly those in low-income countries with limited access to healthcare, are disproportionately affected by the impacts of climate change on disease vectors. These populations often lack the resources to prevent and control outbreaks, leaving them highly susceptible to the devastating consequences of these diseases.
Mitigation and Adaptation Strategies: A Multifaceted Approach
Addressing the threat of climate change’s impact on disease vectors requires a multi-faceted approach encompassing both mitigation and adaptation strategies. Mitigation efforts focus on reducing greenhouse gas emissions to slow the pace of climate change. This includes transitioning to renewable energy sources, improving energy efficiency, and promoting sustainable land use practices. These efforts are essential to reducing the long-term risks posed by climate change to human health.
Adaptation strategies, on the other hand, focus on reducing vulnerability to the unavoidable impacts of climate change. This includes improving disease surveillance systems, enhancing vector control measures, developing and deploying effective vaccines, and strengthening healthcare infrastructure. Early warning systems for predicting outbreaks can also play a vital role in reducing the severity and impact of future epidemics.
Community engagement and education are crucial components of effective adaptation strategies. Empowering communities to understand the risks and implement preventive measures is essential for building resilience to the impacts of climate change on disease vectors.
Research and Monitoring: Filling Knowledge Gaps
Continued research and monitoring are vital for improving our understanding of the complex interactions between climate change and disease vectors. Advanced climate modeling, coupled with detailed epidemiological studies, can help refine predictions of future disease risks and guide the development of effective interventions. Investing in research infrastructure and data collection is crucial for informed decision-making and effective public health policies.
Global collaboration is also essential. Sharing data and best practices across international borders can help strengthen global capacity to address the challenges posed by climate change’s impact on disease vectors. International cooperation is particularly important in addressing the needs of vulnerable populations in low-income countries.
Conclusion: A Call for Urgent Action
The impact of climate change on disease vectors is a significant and growing threat to global health security. The interconnectedness of climate, ecosystems, and human health necessitates a comprehensive and integrated approach to mitigation and adaptation. Urgent action is needed to reduce greenhouse gas emissions, strengthen public health infrastructure, and enhance global collaboration to protect populations from the devastating consequences of climate change-related disease outbreaks. Delaying action will only exacerbate the risks, leading to more frequent, severe, and widespread outbreaks of vector-borne diseases.
The challenge is immense, but the potential benefits of proactive and coordinated action are even greater. By investing in research, implementing effective interventions, and fostering global collaboration, we can mitigate the risks and protect vulnerable populations from the devastating effects of climate change on disease vectors.